Unless you’ve just emerged from the wilderness after several decades, chances are you’ve heard some of the roiling discussions going on across the country concerning the current state of the health care system. Whether it’s presidential candidates working on a policy speech or an individual making home budgeting decisions, implementing a comprehensive health care reform plan continues to be a hot topic.
But while politicians and medical officials across the nation argue the effectiveness of measures like the Affordable Care Act and how to make health care more accessible for the average citizen, some health care providers in Western North Carolina are pursuing the innovative strategy of integrated care in the hope that improving communication among providers and streamlining the availability and type of care patients receive will make accessing and providing care easier and more effective both locally and statewide in the near future.
While several aspects of the overall vision remain in the planning stages—and many challenges lie ahead— a new brick-and-mortar facility in Asheville is already offering several services to the public, with expectations to be fully operational by next March, and the groundwork for improved interaction between health care providers is in the works.
Many services, one patient
The World Health Organization defines integrated care as “the organization and management of health services so that people get the care they need, when they need it, in ways that are user-friendly, achieve the desired results and provide value for money.”
The value and effectiveness of an integrated care model has been explored and expounded upon by many esteemed organizations within the health care universe, including the Mayo Clinic, the American Medical Association, the international consulting firm McKinsey & Co., the Substance Abuse and Mental Health Services Administration, Stanford University, National Committee for Quality Assurance and the U. S. Department of Health and Human Services.
Xpress explored the various facets of integrated care (“The value of patient-centered care,” Jan. 28) earlier this year in its multi-issue Wellness package, in which several local health care and homeopathic providers offered their takes (“Wellness survey participants share their views,” Jan. 28) on what integrated care means and the benefits of approaching patient treatment (“Local practitioners explore medicine’s new frontier,” Jan. 28) from a comprehensive, mind-and-body outlook.
“The idea behind it is to provide the best access to care for individuals in the western part of the state,” says Peter Rives, director of integrated care for Smoky Mountain LME/MCO, a publicly managed care organization that oversees Medicaid, state and local funding and assists in health planning for individuals with mental health, substance use or intellectual and developmental disability health needs. But while Smoky Mountain’s organizational focus may be on mental and behavioral health, the integrated care model would incorporate physical health care providers into the mix, offering comprehensive care options to patients.
“For the individuals that are walking in to these providers, what you get is no wrong door,” says Rives of the long-term value of an integrated care system. “No matter where you show up or what it is that’s affecting you today.”
Rives was hired by Smoky Mountain in June to head the development of the integrated care model and apply it to the existing network of care providers and systems, which spans 23 WNC counties. He says that Smoky Mountain, which partners with health care providers around the area such as RHA Health Services, Asheville Buncombe Community Christian Ministry and Mission Health, is the perfect organization to launch such an overarching reform.

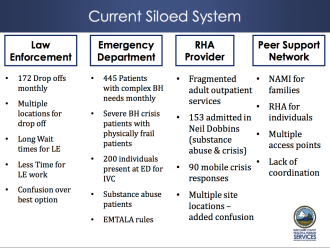
“There’s been a push nationally and internationally to break down the silos that exist within health care and really address the needs of a whole person,” says Rives. “The individuals who access care within Smoky’s provider network for their mental health needs don’t leave their bodies, aches and pains behind at the door.”
Improving the width and depth of response to a patient’s health issues increases the quality of treatment, says Craig Martin, Smoky Mountain LME/MCO’s chief medical officer, who notes that people with chronic mental illness die more than a decade sooner on average than the average North Carolinian. “The reasons for that often times are preventable, and we could help people address them early on, rather than waiting until the end,” he notes.
With this in mind, Smoky Mountain began reforming its care provider network earlier this summer. Plans are in the works to improve communication between health care providers, agencies, patients and their families through a streamlined system of shared records.
“The bottom line is really trying to provide the best quality care we can to the folks we’re serving and doing whatever we can to be integrating and communicating with primary care [providers],” says Sandy Feutz, who works as the vice president of operations for RHA Health Services, one of Smoky Mountain’s partners on the project.
The challenge of the mountains
With that in mind, the question now becomes how Smoky Mountain and its partner agencies will implement such a model in a way that best serves WNC.
“There are models from multiple areas of the country that have a strong evidence base which shows you can save money and prevent chronic conditions from getting worse — and actually reverse course — using some of these integrated care approaches,” Rives says. “Our challenge is to find the right approaches for the unique area that is Western North Carolina.”
One major aspect of this approach is encouraging providers from across mental and physical health specialties to work in tandem and, ideally, under the same roof, to provide care options for a common patient. Smoky Mountain has already made strides in accomplishing this initiative: earlier this month, it assisted in placing a licensed psychiatrist with the Mountain Area Health Education Center and is involved in MAHEC’s Project 1300, which aims to reduce unnecessary emergency department visits by linking up “high-risk” patients suffering from mental illness or substance abuse with primary health care services around the region. The LME/MCO has also established telepsychiatry programs in primary care facilities in Watauga and Avery counties.
However, Rives admits that implementing a complete comprehensive care system requires a fair amount of funding and logistical support to be successful. For those providers not yet ready or able to integrate other forms of care into their practice, Rives says a similar strategy called “coordinated care,” which consists of increasing communication across the traditional divisions of health care, can be effective.
Shelly Foreman, senior director of public affairs for Smoky Mountain, likens this system to the training a doctor receives in medical school, where the student receives basic instruction in a host of different disciplines, with the idea of caring for the whole person rather than a specific area of expertise.
“I think it’s very rewarding to professionals to be able to call on other resources that you feel like you might need and to support what you’re trying to accomplish,” she says. “It makes sense intuitively — we know there is a mind-body connection and that those two things cannot be separated — [and] our system is really trying to work toward that common-sense intuition.”
Integrated care can also provide doctors and primary care providers with a greater pool of knowledge and feedback when making diagnoses, freeing up time and resources for them and reducing costs. “They don’t have to say ‘I’m sorry, I don’t treat that, you’re going to have to go somewhere else or call some other number.'” Rives adds. “They can now say, ‘I’ve got a colleague right down the hall, let me go grab her and she can talk to you about that.’ That’s the power of integrated care.”
A model for success
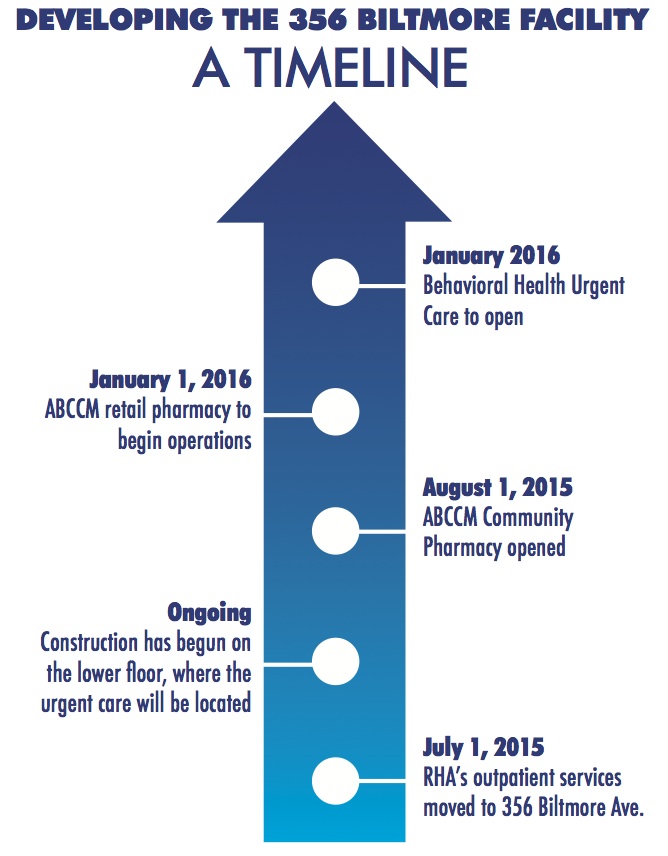
One concrete accomplishment toward the goal of meshing the various offshoots of the health care system is happening at 356 Biltmore Ave., across the street from Mission Hospital. Renovations to the property are underway with the hopes of opening the first fully operational facility-based comprehensive care center in the region by early spring 2016, which will provide an array of physical and mental health resources all in one location.
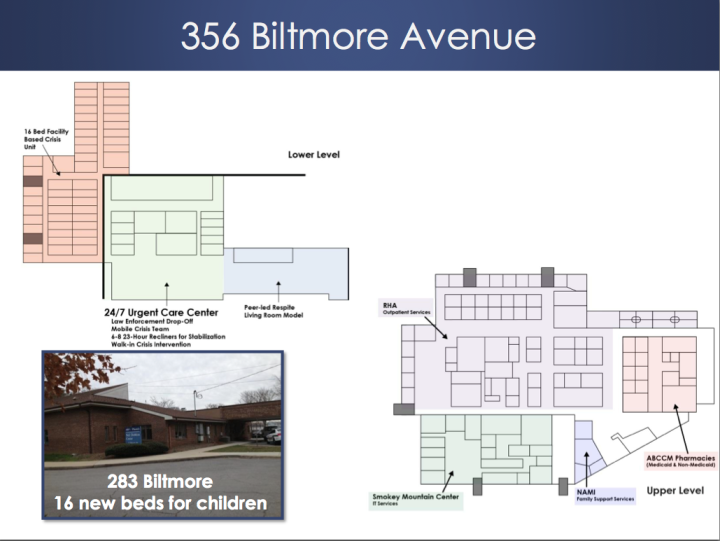
This includes outpatient care provided by RHA and MAHEC (currently operational); an on-site pharmacy operated by ABCCM scheduled to open by Sept. 1; a 24/7 crisis center and detox facility; a peer-respite program where patients can consult with others in recovery; an urgent care-type office for those needing immediate care; and family and mental health resources provided by the Western North Carolina chapter of the National Alliance on Mental Illness, which currently operates out of the building at 356 Biltmore.
In addition to the wide array of services available at the comprehensive care center at 356 Biltmore, the facility will serve those who are underinsured or have no insurance coverage. “Our goals are really about giving a higher quality of care for crisis services, because people who are going to the emergency department aren’t going to get the end goal that’s desired by showing up there,” says Feutz. “Even the medical screenings we’ll do [at 356 Biltmore] are more than a lot of folks who we serve have had in a very long time.”
She adds that having a variety of mental and physical health professionals present and able to collaborate in one location provides the potential to uncover previously undiagnosed conditions in patients.
Foreman says that the facility at 356 Biltmore will provide a “great example” of other projects the care provider is initiating across the region. “There’s not anything quite like this currently in the region,” she says. “What we’re really finding is there’s not anything like it in the state. We may be doing something that’s pretty innovative [nationwide].”
Doctors without borders
While the 356 Biltmore crisis center will be the most visible aspect of the integrated care project, Smoky Mountain and its partner organizations would like to expand this model across the entire region into a comprehensive care network.
To understand how a network like this might work, Foreman says the staff is studying some of the existing partner organizations such as RHA and MAHEC, which envelop a variety of health services across the region. Feutz says that RHA’s approach begins with reaching out to care providers to offer training and feedback on how each professional in the organization’s umbrella can effectively communicate and receive support from other organizations within the network.
“Oftentimes, that reaching out might simply be a letter that says, ‘This person that you serve is also receiving services from us, this our plan, this is how you can reach us, this is your contact person,’ that sort of thing,” says Feutz. “We like to get that conversation started.”
While Smoky Mountain is working on developing an electronic network that will provide a central hub of this data, Martin indicates that variances in the types of records and databases different care providers use for filing present challenges to a streamlined, one-stop information shop. Much of the currently available information comes after a patient has already received services, he says. “We want to try to get things more into the real time.”
Rives reports that there are designs for a statewide health information data exchange as well, but that such a system is more “aspirational” than operational at the current time. “That is a critical component to the future success of this sort of initiative,” he notes, and until that system is up and running, “we in this region have to be really creative [about] how we fund it, how we exchange information.”
Barriers inherent in the system
While optimism over the 356 Biltmore facility and the new initiatives being launched in the coming year runs high, Foreman is quick to acknowledge that barriers to this model are still very real. She says that many of these challenges can be alleviated by educational outreach to patients and their families.
“We want to give consumers and family members information on how they can better understand the relationship between physical and behavioral health and developmental disability issues,” she says, “even things they need to know to ask their provider so they can become more engaged in knowledge of their own health care and the relationship between mind and body.”
Rives says that biggest challenge for Smoky Mountain and health care providers moving forward is that the state health care system remains “bifurcated.” All the Medicaid physical health services are authorized and billed through one route, while behavioral and intellectual or developmental disability services go through another, he explains. Rives adds that while expanding Medicaid coverage is the easiest way to solve this problem, the state legislature has not gone in that direction.
Many communities do offer free health services at clinics across the state, but how long these clinics remain in operation is often anyone’s guess, according to Feutz. “It’s kind of ever-changing. Practices are open for a while and then they’re not, just like any other,” she notes. Feutz notes that part of RHA’s mission in this regard is “staying up-to-date with what the resources are.”
And while the state does have funding in place for indigent populations in need of health care, Foreman says that funding is “a very small resource.” However, she sees the idea of integrated care as posing benefits to the taxpayer as well as the patient. “These things mean cost efficiencies, because the better health people enjoy, the less crisis they have to go through, the more they stay healthier and the more cost-effective the whole system becomes. As a public manager of care, those resources and cost efficiencies can be turned into greater services, more services and more funds for services for people in the community.”
Planning for the future
For now, Smoky Mountain LME/MCO and its partners will continue to refine and tweak their vision of an integrated care system as the January launch date for 356 Biltmore approaches.
Discussions with community members and care providers will continue in earnest as officials attempt to bring this project to fruition, says Foreman. “It’s important to ask ‘Why is this important?'” To that end, she says bringing in experienced professionals such as Rives to oversee the project helps to keep the issues at hand in focus.
And integrated care goes a long way toward dispelling traditional stigmas around mental health and substance abuse issues, he notes. “It can be very refreshing to have other options to access those types of services in a medical setting or in a less stigmatized setting” than one would find in a small community where everyone knows each other.
In essence, Rives says it boils down to the old adage of “working smarter and not harder.”
“By coordinating care, you’re making sure that everybody’s on the same page and everybody has the information they need to provide the best quality care, based on models that we know work and yield good outcomes.”
The task at hand, says Foreman, is figuring out “how can we promote it? How can we support it? How can we build partnerships and support training efforts for our provider network that give them those tools, skills, and contacts needed to do the job more effectively?”




Before you comment
The comments section is here to provide a platform for civil dialogue on the issues we face together as a local community. Xpress is committed to offering this platform for all voices, but when the tone of the discussion gets nasty or strays off topic, we believe many people choose not to participate. Xpress editors are determined to moderate comments to ensure a constructive interchange is maintained. All comments judged not to be in keeping with the spirit of civil discourse will be removed and repeat violators will be banned. See here for our terms of service. Thank you for being part of this effort to promote respectful discussion.